Research article/ Open Access
DOI:10.31488/EJRM.155
Maternal Mortality Associated with Severe Acute Respiratory Syndrome due to COVID-19 in São Paulo, Brazil: Epidemiological Patterns and Associated Risk Factors (2020-2023)
Priscila Cristina João* , Cintia Johnston, Werther Brunow de Carvalho, Edna Maria de Albuquerque Diniz
1. DepartmenDepartment of Pediatrics, Faculty of Medicine University of São Paulo (ICr/HCFMUSP), Brazil
*Corresponding author: : Priscila Cristina João, Faculty of Medicine University of São Paulo (ICr/HCFMUSP) Av. Dr. Enéas Carvalho de Aguiar, 647 - Cerqueira César, São Paulo - SP, 05403-000, Brazil, Tel: +55 11 94553-4951; E-mail: prisjoao@gmail. com.br
Abstract
This study aimed to analyze maternal mortality among pregnant and postpartum women with Severe Acute Respiratory Syndrome (SARS) caused by SARS-CoV-2 in the state of São Paulo, Brazil, between February 2020 and December 2023. This retrospective study of secondary surveillance data from the Influenza Epidemiological Surveillance System (SIVEP-Gripe). A total of 5,640 cases of COVID-19-associated SARS were reported in this population, with the highest concentration observed in 2021 (48.9%)—a period marked by the predominance of the Gamma variant, healthcare system overload, and the initial rollout of maternal vaccination. The overall maternal mortality rate was 6.6% among hospitalized pregnant and postpartum women. Risk factors significantly associated with increased mortality included residence in inland or coastal regions (OR: 1.85; 95% CI: 1.11–3.06), presence of pre-existing comorbidities (OR: 1.78; 95% CI: 1.27–2.51), lack of adequate treatment (OR: 2.1; 95% CI: 1.35–3.03), ICU admission (OR: 6.6; 95% CI: 4.5–9.5), and need for ventilatory support (OR: 3.2; 95% CI: 2.0–5.1). Notably, mortality risk was significantly higher in the postpartum period compared to during pregnancy (OR: 0.36; 95% CI: 0.25–0.51). These findings underscore the profound impact of the COVID-19 pandemic on maternal health in São Paulo, highlighting the urgent need for targeted public health interventions and equitable access to obstetric and intensive care during health emergencies.
Keywords: Maternal mortality, Coronavirus infections, Pregnancy, Puerperium, Severe acute respiratory syndrome, COVID-19
Introduction
The COVID-19 pandemic, caused by the novel coronavirus SARS-CoV-2, rapidly escalated into a global health emergency, placing unprecedented strain on healthcare systems and disproportionately impacting vulnerable populations [1,2]. Since its emergence in late 2019, COVID-19 has resulted in millions of deaths worldwide and has exposed deep-rooted social and structural inequalities in access to healthcare. These disparities have been particularly evident in low- and middle-income countries, which have encountered greater challenges in delivering timely and equitable responses to mitigate the pandemic's effects [3-7].
Pregnant and postpartum women have been identified as a high-risk group for severe COVID-19 outcomes [6-9]. Physiological adaptations during pregnancy and the puerperium-including increased oxygen demand, reduced pulmonary reserve, and immunological modulation-may contribute to heightened vulnerability to complications [10-12]. Evidence indicates higher rates of hospitalization, intensive care unit (ICU) admission, mechanical ventilation, and maternal mortality among pregnant individuals infected with SARS-CoV-2, particularly in settings with limited access to specialized obstetric and critical care services [9-11].
In Brazil, the COVID-19 pandemic had a particularly severe impact on maternal health outcomes [6,8,9]. The state of São Paulo-the country’s most populous-emerged as one of the primary epicenters, reporting high numbers of COVID-19 cases, hospitalizations, and deaths [13,14]. The spread of highly transmissible variants, delayed vaccine rollout for pregnant women, and persistent structural disparities across regions further exacerbated maternal vulnerability. Despite improvements in surveillance systems and clinical management protocols, maternal mortality related to COVID-19 remained a pressing concern, especially during 2021 [6].
In this context, understanding the regional dynamics of maternal mortality associated with COVID-19 is critical to informing targeted public health interventions. This study aimed to analyze mortality rates and associated risk factors among pregnant and postpartum women with Severe Acute Respiratory Syndrome (SARS) caused by SARS-CoV-2 in the state of São Paulo, from February 2020 to December 2023.
Methods
This retrospective study of secondary surveillance data investigated maternal mortality associated with Severe Acute Respiratory Syndrome (SARS) caused by SARS-CoV-2 in the state of São Paulo, Brazil, between February 1, 2020, and December 31, 2023. The analysis was based on secondary data extracted from the Influenza Epidemiological Surveillance Information System (SIVEP-Gripe), a nationwide database coordinated by the Brazilian Ministry of Health in partnership with state and municipal health departments.
Established in 2009, SIVEP-Gripe was expanded during the COVID-19 pandemic to comprehensively capture clinical and epidemiological information on SARS cases, including those linked to SARS-CoV-2 infection. The study population included all pregnant and postpartum women (up to 45 days after delivery) aged 10 to 49 years, residing in the state of São Paulo, who were reported to SIVEP-Gripe with laboratory-confirmed or clinically/epidemiologically diagnosed SARS due to COVID-19. Exclusion criteria encompassed cases with missing or inconsistent data on key outcome variables, particularly regarding survival status.
To address regional disparities in healthcare infrastructure and population density, the state was divided into three geographic categories: "Capital" (São Paulo city), "Metropolitan Region" (38 municipalities surrounding the capital), and "Interior/Littoral" (the remaining 606 municipalities within Health Departments DRS 2–17).The dataset was obtained from the OpenDataSUS platform (https://opendatasus.saude.gov.br), which provides public access to anonymized health surveillance data. Variables extracted for analysis included maternal age (<20, 20–34, ≥35 years), race/ethnicity (White, Black, Other), municipality of residence, gestational trimester (first, second, third), puerperal status, presence of underlying comorbidities (e.g., chronic respiratory or cardiovascular diseases, diabetes, renal disease, immunosuppression, and obesity), ICU admission, use and type of ventilatory support (invasive, non-invasive, or none), COVID-19 vaccination status (available from July 2021), and outcome (survival or death). The gestational trimester was defined based on the gestational age at admission, classified as follows: the first trimester includes the first 12 weeks of pregnancy, the second trimester spans from the 13th to the 26th week, and the third trimester covers from the 27th week until the end of the pregnancy. Missing values were treated as indicative of the absence of the condition, in line with previous methodological approaches used in national studies.
Descriptive statistics were used to characterize the study population, with categorical variables presented as absolute and relative frequencies. Continuous variables were expressed as medians and interquartile ranges, and compared using the Mann-Whitney U test. Categorical variables were compared using Pearson’s chi-square or Fisher’s exact tests, as appropriate. Univariable logistic regression models were employed to estimate odds ratios (ORs) and 95% confidence intervals (CIs) for factors associated with maternal mortality. Variables showing statistical significance (p < 0.05) in univariable analyses were included in multivariable logistic regression models to identify independent predictors of death. All statistical tests were two-tailed, with a significance level set at 5%.
All analyses were conducted using Stata® version 15.1 (StataCorp LLC, College Station, TX, USA). The study was approved by the Research Ethics Committee of the Hospital das Clínicas, Faculty of Medicine, University of São Paulo (approval no. 4.074.841; CAAE: 32615020.1.0000.0068). Given that the research involved the analysis of anonymized, publicly available secondary data, the requirement for informed consent was waived, in accordance with Brazilian ethical standards for human research.
Results
Over the four-year span of the COVID-19 pandemic, a total of 5,460 pregnant and postpartum women were hospitalized due to SARS associated with SARS-CoV-2 infection in the state of São Paulo, Brazil. Of these, 376 maternal deaths were reported, resulting in a case fatality rate of 6.6% among hospitalized cases.
Table 1 presents the demographic and healthcare-related characteristics of maternal deaths due to SARS associated with COVID-19 in São Paulo, categorized by year of notification. The majority of deaths occurred among women aged 20 to 34 years. A statistically significant variation was observed in the distribution of comorbidities over the study period, particularly regarding diabetes mellitus (p = 0.01), immunosuppression (p = 0.02), and, most notably, the absence of pre-existing comorbidities (p < 0.001).
Table 1. Demographic and Healthcare Characteristics of Maternal Deaths Due to SARS-CoV-2 in the State of São Paulo, by Year of Notification.
| Variables, n (%) | n=80 2020 | 2021 n=276 | 2022 n=17 | n=3 2023 | p-value $ | |
|---|---|---|---|---|---|---|
| Age | ||||||
| < 20 years | 6 (7.5) | 12 (4.3) | 3 (17.6) | 1 (33.4) | 0.21 | |
| 20–34 years | 50 (62.5) | 159 (57.6) | 7 (41.2) | 2 (66.6) | 0.40 | |
| ≥ 35 years | 24 (30.0) | 106 (38.4) | 7 (41.2) | - | 0.17 | |
| Ethnicity* | ||||||
| White | 39 (51.3) | 157 (63.6) | 10 (58.8) | 1 (33.4) | 0.19 | |
| Black | 11 (14.5) | 23 (9.3) | 3 (17.6) | - | 0.14 | |
| Other | 26 (34.2) | 67 (27.1) | 4 (23.5) | 2 (66.6) | 0.14 | |
| Gestational trimester | ||||||
| First trimester | 3 (6.8) | 20 (10.7) | 2 (28.6) | 1 (33.4) | 0.25 | |
| Second trimester | 15 (34.1) | 63 (33.9) | 2 (28.6) | 1 (33.4) | 0.43 | |
| Third trimester | 25 (56.9) | 100 (53.8) | 3 (42.8) | 1 (33.4) | 0.37 | |
| Unknown | 1 (2.2) | 3 (1.6) | - | - | - | |
| Comorbidities | ||||||
| Heart disease | 13 (16.3) | 30 (10.8) | 3 (17.6) | 2 (66.6) | 0.18 | |
| Asthma | 2 (2.5) | 10 (3.6) | 1 (5.8) | - | 0.62 | |
| Pulmonary disease | 1 (1.3) | 4 (1.4) | 1 (5.8) | - | 0.75 | |
| Diabetes mellitus | 20 (25.0) | 26 (9.4) | 4 (23.5) | - | <0.001 | |
| Renal disease | 2 (2.5) | 2 (0.7) | 3 (17.6) | - | 0.14 | |
| Obesity | 12 (15.0) | 46 (16.6) | 3 (17.6) | - | 0.72 | |
| Hematological disease | 2 (2.5) | 1 (0.4) | - | - | 0.29 | |
| Neurological disease | 1 (1.3) | 2 (0.7) | - | - | 0.94 | |
| Liver disease | - | 1 (0.4) | - | - | - | |
| Immunosuppressed | 5 (6.3) | 2 (0.7) | 1 (5.8) | - | 0.01 | |
| No comorbidities | 27 (33.7) | 154 (55.8) | 1 (5.8) | 1 (33.4) | <0.001 | |
| Medical care | ||||||
| ICU admission | 64 (80.0) | 196 (71.0) | 14 (82.3) | 2 (66.6) | 0.10 | |
| Invasive mechanical ventilation | 45 (56.3) | 156 (56.5) | 11 (64.7) | 2 (66.6) | 0.85 | |
| Non-invasive ventilation | 17 (21.3) | 84 (30.4) | 1 (5.8) | - | 0.08 | |
* Ethnicity data were not available for all patients. ICU: Intensive Care Unit. Fisher’s exact test was applied to variables with at least one cell containing zero; otherwise, Pearson’s chi-square test was used. $each comparison was conducted independently, and no adjustment for multiple testing was performed; results should be interpreted as exploratory.
A striking finding was the considerable proportion of maternal deaths occurring in the absence of intensive care. A significant percentage of deceased patients had not been admitted to intensive care units (ICU) or had not received invasive mechanical ventilation, indicating critical barriers to timely and adequate care.
Demographic and clinical characteristics associated with increased mortality included advanced maternal age (≥35 years: 36.3% vs. 28.1%; p = 0.04), the presence of at least one comorbidity (51.4% vs. 25.9%; p < 0.001), and occurrence during the second or third trimester of pregnancy (p = 0.01). No statistically significant difference was found with respect to ethnicity (p = 0.74).
In the state of São Paulo, the maternal mortality rate due to SARS associated with COVID-19 between 2020 and 2023 was 6.6% among hospitalized cases. This rate varied over the years, with a notable peak in 2021, reaching 9.9% (Figure1). In 2020 and 2021, the majority of deaths occurred among pregnant women, accounting for 55.0% and 67.4% of cases, respectively. However, in 2022, this pattern reversed, with postpartum women representing 68.8% of the maternal deaths.
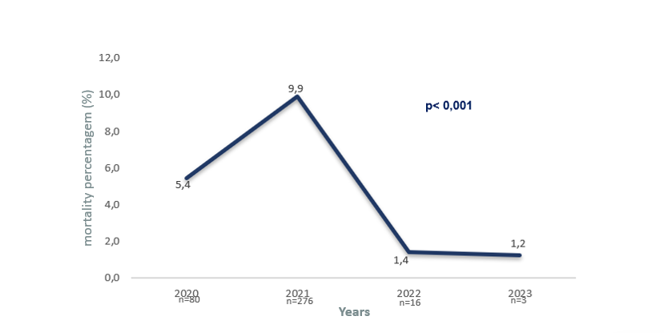
Figure 1:Temporal Trends in Maternal Mortality Rate Due to SARS Associated with COVID-19.
A significant geographic disparity in mortality rates was observed, with the highest proportion of maternal deaths consistently occurring among residents of non-capital municipalities (Interior and Coastal regions). This disparity peaked in 2021 at 66.7% and remained disproportionately high in subsequent years (p < 0.001), as shown in Figure 2. Multivariate logistic regression analysis further confirmed this finding, revealing increased odds of maternal death for women living in these areas (OR: 1.85; 95% CI: 1.11–3.06).
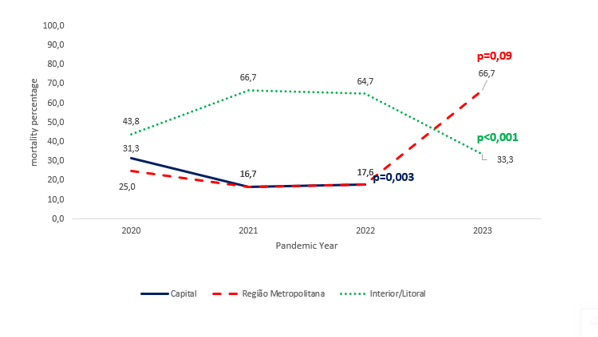
Figure 2:Proportion of Maternal Deaths Due to COVID-19 by Place of Residence.
The need for ICU admission (OR: 6.6; 95% CI: 4.5–9.5) and invasive ventilatory support (OR: 3.2; 95% CI: 2.0–5.1) were strongly associated with increased mortality. However, these associations may also reflect the severity of clinical presentation rather than solely delays in treatment. Nonetheless, the absence of any form of treatment was more common among survivors (21.1%) than among those who died (16.2%), suggesting that under-treatment may have worsened outcomes (p = 0.001).
The introduction of COVID-19 vaccination for this population in 2021 had a clear protective effect. Throughout the study period, the vast majority of maternal deaths occurred among unvaccinated individuals (78.2%; p = 0.001), with an adjusted OR of 2.1 (95% CI: 1.35–3.03) for those who had not received the vaccine (Figure 3).
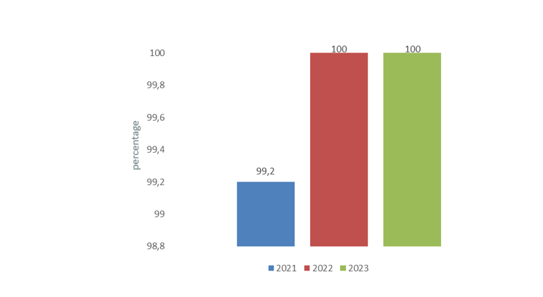
Figure 3:Maternal Mortality and COVID-19 Vaccination Status.
The year-by-year distribution revealed a disproportionate concentration of deaths in 2021 (73.4%; p = 0.008), a period characterized by both higher viral transmissibility and limited vaccine coverage. Maternal status was also associated with divergent outcomes, with postpartum women facing a significantly higher risk of death compared to pregnant women (OR: 0.36; 95% CI: 0.25–0.51), highlighting the increased vulnerability during the puerperium.
Figure 4 presents the multivariate odds ratios for maternal death among hospitalized pregnant and postpartum women, emphasizing 2021 as the year with the highest risk (OR: 1.8; 95% CI: 1.16–2.67), followed by significant associations with regional disparities, the presence of comorbidities, lack of access to treatment, postpartum status, and critical care needs.
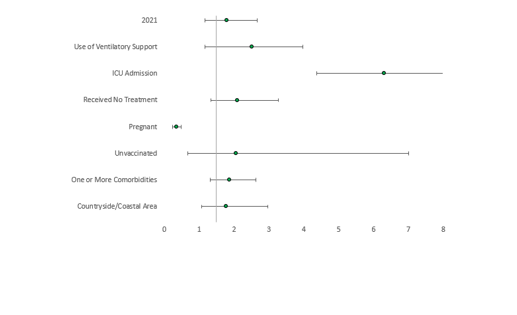
Figure 4:Risk Ratios and 95%Confidence Intervals for Maternal Mortality Rates.
Discussion
The state of São Paulo, the most populous in Brazil, emerged as one of the primary epicenters of the COVID-19 pandemic in the country. Between 2020 and 2023, the overall maternal mortality rate due to SARS associated with COVID-19 was 6.6% among hospitalized pregnant and postpartum women, peaking in 2021. This increase was driven by several factors, including the circulation of the Gamma variant (P.1), which was characterized by high transmissibility and immune evasion capabilities, as well as systemic weaknesses in access to and the quality of obstetric care.
Maternal mortality is a sensitive indicator of socioeconomic conditions and healthcare quality. It rose significantly across all Brazilian states, particularly between March and June 2021. Our study found nearly a twofold increase in mortality risk during this period (OR: 1.8; 95% CI: 1.16–2.67), with a significant predominance of deaths among pregnant women (67.4%). The higher affinity of the Gamma variant for the ACE2 receptor, which is physiologically upregulated during pregnancy, may have contributed to increased clinical severity in pregnant women. The resulting inflammatory storm, endothelial dysfunction, and respiratory failure further exacerbated obstetric outcomes. Similar findings were reported by Gonçalves et al. (2021), who observed more than a twofold increase in maternal mortality in 2021 (OR: 2.6; 95% CI: 2.28–2.97).
The relaxation of social distancing measures, especially toward the end of 2020, also increased pregnant women’s exposure to SARS-CoV-2, thereby contributing to higher mortality rates. This situation was further aggravated by high hospital occupancy rates, which limited the availability of adequate care for pregnant women. However, after the introduction of vaccination for pregnant women in July 2021, a marked decrease in infection and maternal mortality rates was observed, highlighting the protective effect of immunization.omorbidities such as obesity, diabetes, and cardiovascular diseases were strongly associated with increased maternal mortality risk, raising the odds by 1.78 (OR: 1.78; 95% CI: 1.27–2.51). A similar study conducted in Brazil also supports the finding that the presence of these clinical conditions significantly elevates the risk of maternal death.
Obesity, in particular, has been linked to severe maternal morbidity during the antepartum period and can contribute to fatal outcomes due to complications like preeclampsia. These comorbidities often provoke an exaggerated inflammatory response, worsening the clinical condition, complicating treatment, and increasing the likelihood of adverse outcomes. Admission to an ICU increased the risk of maternal death by 6.6 times (OR: 6.6; 95% CI: 4.5–9.5), while the need for ventilatory support raised this risk by 3.2 times (OR: 3.2; 95% CI: 2.0–5.1).
These findings align with the study by Bergantini et al. (2024), which showed that ICU admission doubles the likelihood of maternal mortality. The increased clinical severity of patients requiring intensive care helps explain this elevated risk, as these individuals often present with more critical conditions and are more susceptible to fatal complications. Furthermore, the availability of hospitals equipped with specialized maternal and perinatal care services, including proper infrastructure for managing critically ill pregnant and postpartum women, plays a key role in reducing mortality. A lack of these resources or inadequate facilities can compromise care quality and contribute to higher mortality rates in this vulnerable population.
A concerning finding in this study was the occurrence of significant healthcare failures, with 16.2% of maternal deaths happening without the patients receiving any medical assistance. Similar findings were reported by Takemoto et al. (2020) during the first year of the pandemic, when 15% of women lacked access to ventilatory support, 28% were not admitted to an intensive care unit (ICU), and 36% did not receive intubation or mechanical ventilation [5]. This issue has also been observed in other Latin American countries [31], particularly in Mexico, which, despite having a robust surveillance system, recorded similar rates of inadequate care [30].
This study has some limitations inherent to the use of secondary data from the SIVEP-Gripe system, which should be considered when interpreting the results:
• Underreporting and data inconsistencies: There may have been underreporting of cases and deaths, particularly during the early months of the pandemic, due to limited access to diagnostic testing, delays in case reporting, and the strain on healthcare systems. Additionally, the quality and completeness of data may vary across different municipalities.
• Limitations in distinguishing between direct and indirect causes of death: It was not possible to accurately differentiate deaths directly caused by SARS-CoV-2 infection from those resulting from obstetric complications exacerbated by the infection. This could lead to either an overestimation or underestimation of the COVID-19-related maternal mortality rate.
Conclusion
In the state of São Paulo, a major epicenter of the COVID-19 pandemic in Brazil, the overall maternal mortality rate due to COVID-19–related SARS was 6.6%, peaking in 2021. This surge coincided with an overwhelmed healthcare system, the circulation of more transmissible and aggressive viral variants, and limited vaccine access during the early stages of the pandemic.
The distribution of cases and deaths revealed regional disparities, with women in inland and coastal areas facing higher mortality risks, highlighting significant structural inequalities in healthcare access. Maternal mortality was associated with factors such as pre-existing comorbidities, lack of appropriate treatment or vaccination, ICU admission, need for ventilatory support, and the postpartum period.
Abbreviations
COVID-19: Coronavirus Disease 2019; SARS: Severe Acute Respiratory Syndrome; SARS-CoV-2: Severe Acute Respiratory Syndrome Coronavirus 2; ICU: Intensive Care Unit; OR: Odds Ratio; CI: Confidence Interval; SIVEP-Gripe: Influenza Epidemiological Surveillance Information System; ECA2: Angiotensin-Converting Enzyme 2.
References
1. World Health Organization (WHO). WHO Director-General's statement on IHR Emergency Committee on Novel Coronavirus (2019-nCoV), 30 January 2020 [Internet]. Geneva: WHO; 2020 [citado 2024 abr 4]. Disponível em: https://www.who.int/director-general/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov)
2. Gonçalves BMM, Franco RPV, Rodrigues AS. Maternal mortality associated with COVID-19 in Brazil in 2020 and 2021: Comparison with non-pregnant women and men. PLoS One. 2021 Dec 21;16(12):e0261492. doi: 10.1371/journal.pone.0261492. Erratum in: PLoS One. 2023 Nov 15;18(11):e0294703. doi: 10.1371/journal.pone.0294703. PMID: 34932589; PMCID: PMC8691656.
3. Pollard CA, Morran MP, Nestor-Kalinoski AL. The COVID-19 pandemic: a global health crisis. Physiol Genomics. 2020 Nov 1;52(11):549-557. doi: 10.1152/physiolgenomics.00089.2020. Epub 2020 Sep 29. PMID: 32991251; PMCID: PMC7686876.
4. Organização Pan-Americana da Saúde (OPAS). Atualização epidemiológica: doença do coronavírus (COVID-19) [Internet]. Washington (DC): OPAS/OMS; 2021 jul [citado 2021 out 23]. Disponível em: https://www.paho.org/es/documentos/actualizacion-epidemiologica-enfermedad-por-coronavirus-covid-19-22-julio-2021
5. Francisco RPV, Lacerda L, Rodrigues AS. Obstetric Observatory BRAZIL - COVID-19: 1031 maternal deaths because of COVID-19 and the unequal access to health care services. Clinics (Sao Paulo). 2021 Jun 28;76:e3120. doi: 10.6061/clinics/2021/e3120. PMID: 34190858; PMCID: PMC8221555.
6. Takemoto MLS, Menezes MO, Andreucci CB, Nakamura-Pereira M, Amorim MMR, Katz L, et al. The tragedy of COVID-19 in Brazil: 124 maternal deaths and counting. Int J Gynaecol Obstet. 2020 Oct;151(1):154-156. doi: 10.1002/ijgo.13300. Epub 2020 Jul 29. PMID: 32644220; PMCID: PMC9087660.
7. Orellana J, Jacques N, Leventhal DGP, Marrero L, Morón-Duarte LS. Excess maternal mortality in Brazil: Regional inequalities and trajectories during the COVID-19 epidemic. PLoS One. 2022 Oct 20;17(10):e0275333. doi: 10.1371/journal.pone.0275333. PMID: 36264994; PMCID: PMC9584504.
8. Karimi L, Vahedian-Azimi A, Makvandi S, Sahebkar A. A systematic review of 571 pregnancies affected by COVID-19. Adv Exp Med Biol. 2021;1321:287-298. doi: 10.1007/978-3-030-59261-5_26. PMID: 33656734.
9. Joseph NT, Wylie BJ. Maternal deaths in Brazil from severe COVID-19 respiratory disease: time for a global commitment to ending health disparities. BJOG. 2020 Dec;127(13):1627. doi: 10.1111/1471-0528.16521. Epub 2020 Oct 8. PMID: 32959491; PMCID: PMC7537235.
10. Hojo-Souza NS, Guidoni DL, Da Silva CM, De Souza FSH. A temporal study of Brazilian pregnant and postpartum women vulnerability for COVID-19: Characteristics, risk factors and outcomes. Lancet Reg Health Am. 2022 May;9:100197. doi: 10.1016/j.lana.2022.100197. PMID: 35156076; PMCID: PMC8824236.
11. Smith ER, Oakley E, Grandner GW, et al. Clinical risk factors of adverse outcomes among women with COVID-19 in the pregnancy and postpartum period: a sequential, prospective meta-analysis. Am J Obstet Gynecol. 2023;228(2):161-177. doi: 10.1016/j.ajog.2022.08.038.
12. Lassi ZS, Ali A, Das JK, Salam RA, Padhani ZA, Irfan O, et al. A systematic review and meta-analysis of data on pregnant women with confirmed COVID-19: Clinical presentation, and pregnancy and perinatal outcomes based on COVID-19 severity. J Glob Health. 2021;11:05018. doi: 10.7189/jogh.11.05018.
13. Dashraath P, Wong JLJ, Lim MXK, Lim LM, Li S, et al. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am J Obstet Gynecol. 2020 Jun;222(6):521-531. doi: 10.1016/j.ajog.2020.03.021.
14. Prefeitura de São Paulo. Painel COVID-19 - Município de São Paulo [Internet]. São Paulo: Prefeitura de São Paulo; [citado 2022 mar 25].
15. Lorenz C, Ferreira PM, Masuda ET, Lucas PCC, Palasio RGS, Nielsen L, et al. COVID-19 in the state of São Paulo: the evolution of a pandemic. Rev Bras Epidemiol. 2021 Sep 6;24:e210040. doi: 10.1590/1980-549720210040. PMID: 34495193.
16. Coutinho R, Marquitti F, Ferreira L, Borges M, Da Silva R, Canton O, et al. Model-based estimation of transmissibility and reinfection of SARS-CoV-2 P.1 variant. Commun Med (Lond). 2021;1:48. doi: 10.1038/s43856-021-00048-6.
17. Akkız H. The biological functions and clinical significance of SARS-CoV-2 variants of concern. Front Med (Lausanne). 2022;9:849217. doi: 10.3389/fmed.2022.849217.
18. Calvert C, John J, Nzvere FP, Cresswell JA, Fawcus S, et al. Maternal mortality in the COVID-19 pandemic: findings from a rapid systematic review. Glob Health Action. 2021 Oct 26;14(sup1):1974677. doi: 10.1080/16549716.2021.1974677. PMID: 35377289; PMCID: PMC8986253.
19. da Silva Bueno LA, Ribeiro MAL, Martins CB, de Abreu LC, de Almeida AD Jr, et al. Describing trends in maternal mortality in the State of São Paulo, Brazil, from 2009 to 2019. Healthcare (Basel). 2023 Sep 12;11(18):2522. doi: 10.3390/healthcare11182522. PMID: 37761720; PMCID: PMC10530346.
20. Orellana JDY, Leventhal DGP, Flores-Quispe MDP, Marrero L, Jacques N, Morón-Duarte LS, et al. Impact of the COVID-19 pandemic on excess maternal deaths in Brazil: A two-year assessment. PLoS One. 2024 Apr 2;19(4):e0298822. doi: 10.1371/journal.pone.0298822. PMID: 38564620; PMCID: PMC10986939.
21. Xavier MO, Amouzou A, Maïga A, Akseer N, Huicho L, Matijasevich A. The impact of the COVID-19 pandemic on trends in stillbirths, under-5 and maternal mortality in Brazil: Excess deaths and regional inequalities. J Glob Health. 2023 Sep 30;13:06040. doi: 10.7189/jogh.13.06040. PMID: 37772786; PMCID: PMC10540663.
22. Narang K, Enninga EA, Gunaratne MD, Ibirogba ER, Trad AT, Elrefaei A, et al. SARS-CoV-2 infection and COVID-19 during pregnancy: A multidisciplinary review. Mayo Clin Proc. 2020;95(8):1750-1765. doi: 10.1016/j.mayocp.2020.05.011.
23. Phoswa WN, Khaliq OP. Is pregnancy a risk factor of COVID-19?. Eur J Obstet Gynecol Reprod Biol. 2020;252:605-609. doi: 10.1016/j.ejogrb.2020.06.058.
24. Testa CB, de Godoi LG, Monroy NAJ, Bortolotto MRFL, Rodrigues AS, Francisco RPV. Impact of Gamma COVID-19 variant on the prognosis of hospitalized pregnant and postpartum women with cardiovascular disease. Clinics (Sao Paulo). 2024 Aug 8;79:100454. doi: 10.1016/j.clinsp.2024.100454. PMID: 39121513; PMCID: PMC11363992.
25. Scheler CA, Discacciati MG, Vale DB, Lajos GJ, Surita F, Teixeira JC. Mortality in pregnancy and the postpartum period in women with severe acute respiratory distress syndrome related to COVID-19 in Brazil, 2020. Int J Gynaecol Obstet. 2021 Dec;155(3):475-482. doi: 10.1002/ijgo.13804. Epub 2021 Jul 16. PMID: 34185314; PMCID: PMC9087770.
26. Ribeiro MR, Silva MAP, Prates LFL, Oliveira RR, Carvalho MDB, Pelloso SM. Factors associated with COVID-19 death in pregnant women hospitalized in Intensive Care Units. Rev Bras Enferm. 2024 Aug 26;77(5):e20230172. doi: 10.1590/0034-7167-2023-0172. PMID: 39194128; PMCID: PMC11346909.
27. Carvalho-Sauer R, Costa MDCN, Teixeira MG, Flores-Ortiz R, Leal JTFM, Saavedra R, et al. Maternal and perinatal health indicators in Brazil over a decade: assessing the impact of the COVID-19 pandemic and SARS-CoV-2 vaccination through interrupted time series analysis. Lancet Reg Health Am. 2024 May 23;35:100774. doi: 10.1016/j.lana.2024.100774. PMID: 38828284; PMCID: PMC11143910.
28. Poorolajal J, Jenabi E. The association between body mass index and preeclampsia: a meta-analysis. J Matern Fetal Neonatal Med. 2016 Nov;29(22):3670-6. doi: 10.3109/14767058.2016.1140738. Epub 2016 Feb 12. PMID: 26762770.
29. Torres-Torres J, Martinez-Portilla RJ, Espino-Y-Sosa S, et al. Comorbidity, poverty and social vulnerability as risk factors for mortality in pregnant women with confirmed SARS-CoV-2 infection: analysis of 13 062 positive pregnancies including 176 maternal deaths in Mexico. Ultrasound Obstet Gynecol. 2022;59(1):76-82. doi:10.1002/uog.24797.
30. Bergantini LS, Ichisato SMT, Salci MA, et al. Factors associated with hospitalizations and deaths of pregnant women from Paraná due to COVID-19: a cross-sectional study. Rev Bras Epidemiol. 2024;27:e240005. Published 2024 Feb 5. doi:10.1590/1980-549720240005.
31. Lumbreras-Marquez MI, Campos-Zamora M, Lizaola-Diaz de Leon H, Farber MK. Maternal mortality from COVID-19 in Mexico. Int J Gynaecol Obstet. 2020 Aug;150(2):266-267. doi: 10.1002/ijgo.13250. Epub 2020 Jun 16. PMID: 32473603.
Received:February 03, 2025;
Accepted: February 27, 2025;
Published: March 04, 2025.
To cite this article : João PC, Johnston C, de Carvalho WB, Diniz EMA. Maternal mortality associated with severe acute respiratory syndrome due to COVID-19 in São Paulo, Brazil: epidemiological patterns and associated risk factors (2020–2023). Eur J Respir Med. 2025; 7(1): 481- 486. doi: 10.31488/EJRM.155.
© The Author(s) 2025. This is an open access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/).
